The Benefits of Epilepsy Surgery in Tuberous Sclerosis: A Case Report
DOI:
https://doi.org/10.46900/apn.v7i2.294Keywords:
Epilepsy Surgery, Tuberous sclerosis, Tubers, Epilepsy, lesionectomyAbstract
Introduction/Background: Epilepsy affects millions worldwide, with about one-third of patients remaining drug-resistant despite optimal medical therapy. In tuberous sclerosis complex (TSC), refractory epilepsy is common and severely impacts quality of life. Surgery targeting epileptogenic tubers offers a potential curative approach, contrasting with palliative options like callosotomy.
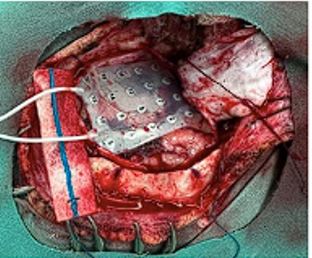
Case Presentation: A 6-year-old girl with TSC presented with daily drug-resistant focal and generalized seizures. MRI revealed multiple cerebral tubers, with EEG identifying a dominant epileptogenic focus in the left temporal lobe. After multidisciplinary evaluation, the patient underwent left temporal craniotomy and lesionectomy, guided by intraoperative electrocorticography. Postoperative monitoring showed no epileptiform activity. Seizure frequency reduced by 50% immediately postoperatively, reaching remission by one month. At one year, she remained seizure-free with reduced antiepileptic therapy and showed cognitive improvements.
Conclusions: Targeted tuber resection effectively controlled seizures and enhanced quality of life, avoiding more invasive palliative procedures. Careful preoperative evaluation to identify dominant epileptogenic foci is critical. Lesionectomy offers superior long-term outcomes over palliative options like callosotomy in selected TSC patients, supporting a tailored surgical approach based on detailed neuroimaging and electrophysiological data.
Downloads
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Eduardo Trejo Olguin, Samuel Pérez Carranza, Samuel Pérez Cárdenas, Estefanía Villarreal Garza, Ana Luisa Carreón, José Ascención Arenas Ruíz, Angel R. Martìnez Ponce de León

This work is licensed under a Creative Commons Attribution 4.0 International License.

When publishing in Archives of Pediatric Neurosurgery journal, authors retain the copyright of their article and agree to license their work using a Creative Commons Attribution 4.0 International Public License (CC BY 4.0), thereby accepting the terms and conditions of this license (https://creativecommons.org/licenses/by/4.0/legalcode).
The CC BY 4.0 license terms applies to both readers and the publisher and allows them to: share (copy and redistribute in any medium or format) and adapt (remix, transform, and build upon) the article for any purpose, even commercially, provided that appropriate credit is given to the authors and the journal in which the article was published.
Authors grant Archives of Pediatric Neurosurgery the right to first publish the article and identify itself as the original publisher. Under the terms of the CC BY 4.0 license, authors allow the journal to distribute the article in third party databases, as long as its original authors and citation details are identified.